
Partial shoulder replacement, also called shoulder hemiarthroplasty is a surgical procedure during which the upper bone in the arm (humerus) is replaced with a prosthetic metal implant, whereas the other half of the shoulder joint (glenoid or socket) is left intact. This surgical procedure is indicated in severe, persistent conditions of shoulder osteoarthritis in which the only the humeral head or ball of the joint is damaged. Osteoarthritis is a degenerative condition in which the cartilage that allows smooth movement in the joints wears away causing the adjacent bone to rub against each other resulting in pain and stiffness. In such conditions, replacement of the damaged portion of the humerus will reduce the friction as bone ends can no longer come in contact and thus relieve pain.
Surgery remains as a sole treatment option when all possible conservative means of treatment such as rest, anti-inflammatory medications, physical therapy have been ineffective in resolving your symptoms. While the procedure may relieve your pain and other symptoms, there may also be associated risks and complications as with any major surgery.
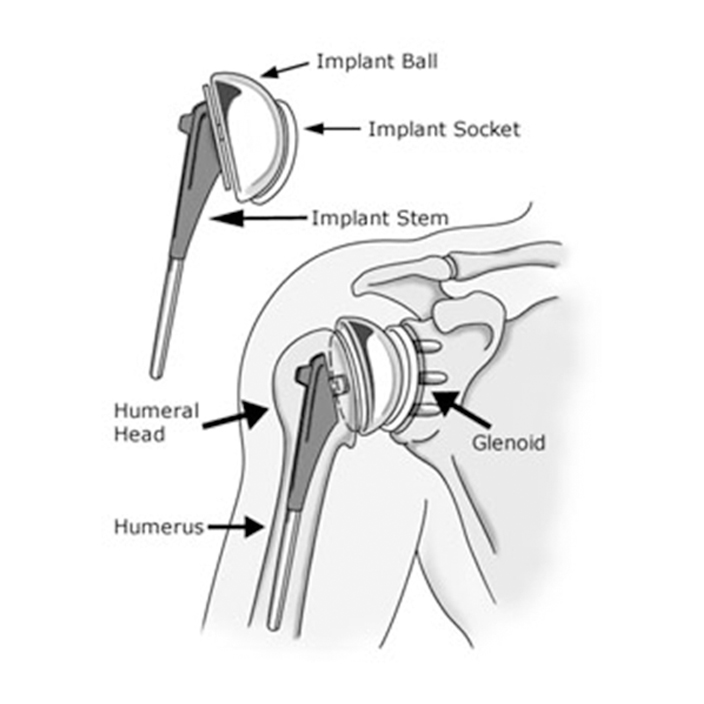
The actual surgery involves replacing the damaged humeral head (or joint “ball”) with a metal ball, and putting a new smooth plastic surface on the glenoid (called the “socket”). Metal on plastic surfaces (rather than metal on metal) are the hallmark of virtually all shoulder replacement implant systems. Partial shoulder replacement (or hemi-replacement) may also be indicated with certain severe shoulder fractures of the humeral head. This technique requires the replacement of the ball component only.
For many shoulder conditions involving the surrounding ligaments, muscles and tendons, such as a torn or diseased rotator cuff or a labral tear, a minimally invasive shoulder arthroscopy procedure is frequently recommended, and they are among the most common and frequently indicated shoulder procedures. Total shoulder replacement, however, requires open surgery, with an incision along the front of the shoulder and upper arm.

The surgeon begins by separating the deltoid and pectoral muscles, accessing the shoulder in a largely nerve-free area to minimize nerve damage. The shoulder is covered by the rotator cuff, which must be opened by cutting one of the anterior (front) rotator cuff muscles. This “opens the door,” allowing the surgeon to view and manipulate the arthritic parts of the shoulder ball and socket.
After the arthritic sections have been removed, the surgeon inserts the implant socket, ball, and stem components, closes and stitches the rotator cuff muscle, and stitches and cleans the incision, after which a bandage is applied as a temporary covering.
Total shoulder arthroplasty is a highly beneficial surgical procedure intended to reduce pain and restore mobility in patients with end stage shoulder arthritis, and occasionally after certain severe shoulder fractures. In most cases, non-operative measures such as medication, injections, and gentle physical therapy are considered prior to deciding on surgery.
It is important to understand that proper and extensive post-operative rehabilitation is a key factor in achieving the maximum benefit of shoulder replacement surgery. With this in mind, TSA is generally considered to be as successful in relieving pain as total hip or knee replacement.
After one year, 95% of TSA patients enjoy pain-free function, which enables them to exercise the shoulder area sufficiently to promote restoration of strength and motion. Because of this, most patients successfully return to the activities they enjoy, making the procedure a highly valued choice for a wide variety of patients suffering from significant shoulder pain due to cartilage loss.