
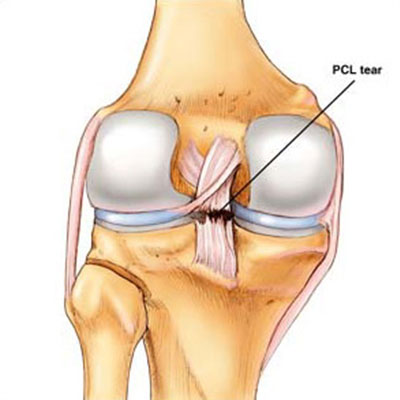
The posterior cruciate ligament, or PCL, is the strongest ligament of the knee. While the anterior cruciate ligament, or ACL is injured more often than the PCL and is more commonly discussed, PCL injuries account for more than 20% of reported knee injuries. Because the ACL sits just in front of the PCL, injuries to the PCL are commonly missed and left undiagnosed.
The posterior cruciate ligament's most important function is to prevent posterior translation of the knee at higher knee flexion angles. Thus, patients commonly complaining of problems with deceleration, problems going down stairs and inclines or general twisting, turning or pivoting activities.
PCL injuries are classified according to the amount of injury to the functional ligament:
In general, Dr. B R Bagaira will perform a PCL reconstruction on all injuries that present themselves as a grade III. In a higher level athlete, it may be recommended to proceed with a PCL reconstruction sooner because the results of acute reconstructions are much better than chronic reconstructions.
When Dr. B R Bagaira does find that a patient needs a surgical PCL reconstruction, he thoroughly assesses the patient to see if there is a concurrent injury. In our hands, approximately 90% of patients who have a symptomatic PCL tear limiting their function also have a posterolateral corner, posteromedial injury or other associated injury. Thus, the incidence of isolated PCL reconstructions in our own series is approximately 10% of the total PCL reconstructions performed.
Our surgical rehabilitation technique for a surgical PCL reconstruction is a double bundle reconstruction with allografts. We use a double bundle reconstruction because historically, the results of PCL reconstruction in the literature have been less than ideal. Dr. B R Bagaira participated in an international symposium of PCL specialists in Florence, Italy in November 2002. At this symposium, all the current anatomy, biomechanics, clinical outcomes and diagnostic methods for PCL ligament injuries and PCL tears were closely reviewed. It was felt, at that point, the outcomes for PCL reconstructions were less than ideal and it was recommended that newer reconstruction and rehabilitation techniques be evaluated. In addition, it was felt rehabilitation had a much stronger effect on the results of a PCL reconstruction compared to an ACL reconstruction and a rehabilitation program was established to maximize patient outcomes.
Dr. B R Bagaira has found that a double bundle PCL reconstruction has been extremely effective in restoring knee stability back to the patient both objectively with PCL stress x-rays as well as subjectively based on patients independently evaluating their outcome scores.
Dr. B R Bagaira's surgical PCL reconstruction technique involves the creation of a closed socket tunnel in the femur for both the anterolateral and posteromedial bundles of the PCL. The graft is fixed in that location and pulled distally down the tibia. The anterolateral bundle is fixed at 90° of knee flexion with an anterior force on the knee and distal traction on the graft. After the anterolateral bundle is fixed to the tibia at 90° of knee flexion, the posteromedial bundle is next fixed in full extension.
Postoperatively, we allow patients to initiate prone knee flexion at 0-90° on day one. The patients use a PCL brace, preferably a PCL Rebound brace, for 6 months postoperatively at all times, except to shower or change clothes, to reduce the posterior gravitational stress to the knee. We also recommend that high level athletes utilize a PCL Rebound brace at least through the completion of the first competitive season after the PCL reconstruction to unload the PCL graft and protect it while it remodels.
We have found that our rehabilitation program, which may be considered aggressive by other treatment centers, has not resulted in any of our grafts stretching out over time and has demonstrated a much quicker return of knee motion, decreased risk of knee stiffness and higher level of function.